CHEMOTHERAPY – INTRODUCTION
General Introduction :
Chemotherapy can be defined as “the use of chemical compounds in the treatment of infectious diseases, so as to destroy offending parasites or organisms without damaging the host tissues”.
The history of chemotherapy can be discussed in three periods as :
The various events, developments, major contribution to chemotherapy are as listed below :
Significance of Various Terms Used in Chemotherapy :
Chemotherapeutic index : According to Ehrlich, substances used as anti-infectives, should produce greater effects on parasites (maximum parasitotropic) and minimum effects on host cells and tissues (minimum organotropic). Such anti-infective agents are defined as ‘desirable’ and posses a favourable chemotherapeutic index, which can be represented as :
Chemotherapeutic index (C.I) = Maximum tolerated dose / Minimum curative dose
Taking into consideration the various routes of administration, different hosts, the above formula is modified as :
Chemotherapeutic index (C.I) = L.D. 0.1 / C.D. 99.9
where,
L D. 0.1. = a dose which will kill all animlas except 0.1%.
C D. 99.9 = dose which cures all animals except 0.1%.
This index indicates margin of safety of anti-infective agents.
General Mechanism of Action of Anti-infective Agents :
The various chemotherapeutic, anti-bacterial agents, used in therapy, act by either of following mechanism :
URINARY ANTISEPTICS
Introduction / Pathophysiology :
Urinary tract infection is defined as a condition characterized by presence of actively multiplying bacteria in the urinary bladder.
When 100,000 or more organisms are present in 1 ml of urine in two separately tested samples, then it is the condition referred to as urinary tract infection. Usually during infection, along with bacteria, white cells also appear.
The clinical conditions informing urinary tract infection are :
URINARY TRACT ANTISEPTICS
Definition :
These are pharmacological agents, which when administered, inhibit the growth of causative organisms of urinary tract infection. Because these agents act locally on kidneys, urinary bladder and uterus. They are called as urinary tract antiseptics.
Classification :
Mechanism of Action :
The pharmacological agents, which are used as urinary antiseptics, when administered get concentrated in the renal tubules and effectively inhibit the growth of the infection causing organisms.
Adverse / Side Effect :
Gastro-intestinal tract upset is very common.
Preparation / Dose :
|
Drug |
Trade name |
Dose |
|
1. Nitrofurantoin |
Furadantin |
100 mg / 6 hr. with food |
|
2. Nalidixic acid |
Gramoneg |
1 gm four times / day |
|
3. Nitrofurazone |
Furacin |
0.2% concentration available as ointment, cream |
|
4. Methenamine |
Mandelamine |
1 gm four times / day |
|
5. Oxolinic acid |
- |
750 mg two times / day oral |
|
6. Furazolidone |
Furoxone |
100 mg 3 times/day for 5 days |
SULFONAMIDES
Definition :
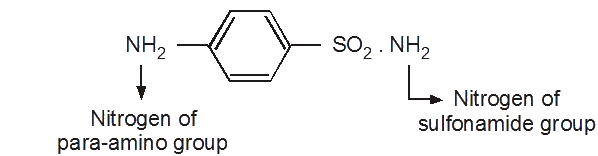
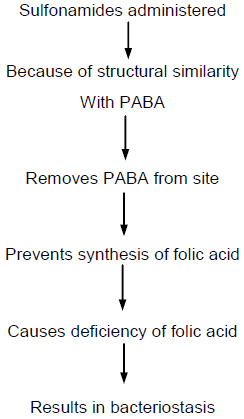
The antimicrobial compounds containing a sulfonamide – SO2NH2 group are called as sulfonamides.
Classification :
Sulfonamides are classified as follows :
Anti-bacterial Spectrum :
Sulfonamides are effective against Gram positive and Gram negative organisms like :
Mechanism of Action :
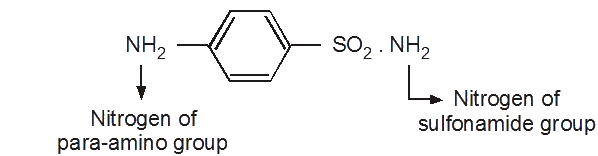
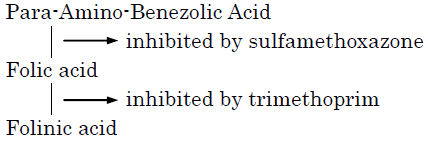
Folic acid derived from Para-amino-benzoic acid is essential for growth and multiplication of microorganism.
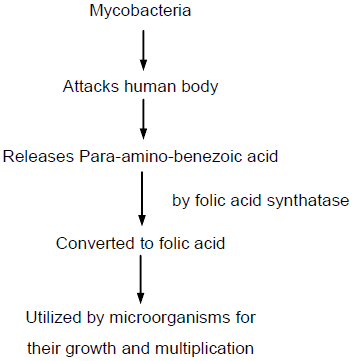
Sulfonamides inhibit folic acid synthetase enzyme; and because of its structural resemblance to para-amino-benzoic acid, removes PABA from the site and inhibits conversion of Para-amino-benzoic acid to folic acid, by attaching to the site.
Because of deficiency of folic acid, microorganism cannot multiply and grow. Thus, growth and multiplication of microorganism stops.
This is termed as ‘bacteriostatic’ action of sulfonamide. Schematically it can be represented as follows :

Absorption, Fate, Excretion :
Sulfonamides used for systemic purposes are well absorbed. The main site of absorption is the small intestine.
In the blood, these drugs are loosely bound to plasma proteins.
Free, acetylated sulfonamides are mainly excreted in urine.
Adverse / Side Effects :
a. Sulfonamides cause renal complications.
In the presence of acidic urine, the acetylated form of sulfonamide is precipitated in collecting tubules and calyces. This causes renal irritation, obstruction to urinary flow, crystaluria, albuminuria, haematuria, oliguria and anuria.
These renal complications can be minimized by
b. On blood system sulfonamides causes agranulocytosis thrombocytopenia.
|
Drug |
Trade names |
Oral dose |
|
Sulfadiazine |
Gantrisin |
2 – 4 gm orally / 6 hr. |
|
Sulfisoxazole |
Gentanol |
2 – 4 gm orally / 6 hr. |
|
Sulfamethoxy pyridazine |
Lederkyn medicil |
Initially 1 gm followed by 0.5 g daily. |
|
Succynyl sulfathiazole |
Sulfasuxidine |
10 – 20 g daily divided dose. |
|
Pthalyl sulfathiazole |
Sulfathalidine |
10 g daily divided dose. |
|
Sulfacetamide |
Albucid |
10 to 30%, 1 or 2 drops in both eyes every four hours. |
Clinical Application / Therapeutic Uses :
Contraindications :
Sulfonamides should be not used (contraindicated) in patients :
Sulfonamide Interaction :
Sulfa Combination :
Clinical Application / Therapeutic Uses :
Adverse / Side Effect :
It is postulated that trimethoprim may increase the gastro-intestinal and haematological toxicity of sulphamethoxazole.
Interactions :
Preparation / Dose :
Trimethoprim, sulfamethoxazole are combined with each other in a ratio 1 : 5. Accordingly the various preparations available are :
|
Combination |
Trade names |
Dose |
|
Trimethoprim 80 mg + Sulfamethoxazole 400 mg |
Septran Bactrim, supristol |
1 / 2 tablets for 14 days. |
|
Paediatric tablets – Trimethoprim – 20 mg + Sulfamethoxazole – 100 mg |
– |
1 / 2 tablets |
|
Trimethoprim 90 mg + Sulfadiazene 410 mg |
Aubril |
1 tablet twice / day |
ANTIBIOTICS
These are chemical compounds produced by living microorganisms like bacteria, fungi and actinomycetes, which at high dilutions, are capable of inhibiting or killing bacteria and other microorganisms.
Potency :
It is defined as activity per milligram of a chemotherapeutic agent and is expressed on the basis of “minimum inhibitory concentration, which is capable of inhibiting the multiplication of one of the susceptible microorganisms”.
Bacteriostatic Activity :
It is defined as “ability of a compound to inhibit growth and multiplication of micro-organisms” e.g. chloramphenicol, erythromycin, tetracycline, sulphonamides etc.
Bactericidal Activity :
It is defined as ability of a compound to kill microorganism.
e.g. penicillins, cephalosporins, vancomycin etc.
Antibacterial Spectrum :
This refers to the range of activity of a compound.
Usually activity of a compound is expressed either as broad-spectrum or narrow -spectrum.
PENICILLIN
Definition :
Antibiotics are chemical substances derived from various species of microorganisms, such as fungi, actinomycetes, bacteria and in higher concentrations suppress growth of other microorganism.
Penicillin is one of the most important antibiotics.
Source :
It is extracted from the mould penicillium notatum.
Structure :
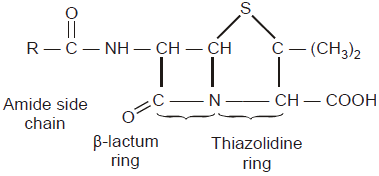
Penicillins represent a large group of antimicrobial agents, consisting of a fundamental nucleus, 6 – Amino – Penicillanic – acid (6 – APA) having a Beta lactum ring.
Classification :
Mechanism of Action :
Penicillins act by interfering with the synthesis of the cell wall mucopeptide of gram-postive cocci. This makes the cell membrane of the organism vulnerable to damage by solutes in the surrounding medium (plasma).
Thus, penicillins are bactericidal drugs and are effective mainly against multiplying organisms.
Antibacterial Spectrum :
Penicillins are mainly effective against Gram-positive and Gram-negative cocci. Streptococci, staphylococci, Gonococci, pneumococci, meningococci are sensitive to penicillin.
Absorption, Fate, Excretion :
Penicillin G, i.e. benzyl penicillin, is inactivated by gastric acid, when orally administered.
Hence, as its absorption is inadequate and irregular, benzyl penicillin is administered by intramuscular route.
Penicillin is widely distributed in the body. It crosses the placental barrier.
Penicillin is eliminated by the kidneys while small amounts appear in bile, milk and saliva.
Co-administration of probenecid delays rapid excretion of penicillin. It competes with penicillin for tubular transport and can raise plasma-penicillin level. The normal dose of probenecid, which is known to increase plasma penicillin level, is 0.5 g six hourly.
Adverse / Side Effects :
Preparation / Dose :
|
1. Benzyl penicillin |
Penicillin G, I.P., injection |
500,000 units per ml intramuscular |
|
2. Phenoxy methyl penicillin |
Penicillin V |
250 mg orally six hourly |
Clinical Application / Therapeutic Uses :
Test for Detection of Penicillin Allergy :
Skin test :
Treatment for Anaphyplactic Shock :
The hypersensitivity reaction produced by penicillin, referred to as anaphylactic shock, can be treated by using following pharmacological agents :
STREPTOMYCIN
AMINOOGLYCOSIDE ANTIBIOTIC – STREPTOMYCIN
Definition :
These are the antibiotics composed of aminosugars, connected by glycosidic linkage. Streptomycin is obtained from streptomyces griseus.
Antibacterial Spectrum :
Streptomycin is effective against M.tuberculosis, Shigella species, Brucella, H. Influenzae, H.ducreyii, Nocardia etc. Streptomycin is more effective in alkaline pH (7 – 8) than acidic pH.
Mechanism of Action :
Ribosomes prepare enzymes under messenger RNA.
It is believed that streptomycin combines with bacterial ribosome, interferes with messenger – Rna combination and compels ribosomes to prepare wrong amino acids sequence, which results in destruction of bacterial cell.
Streptomycin may be bactericidal or bacteriostatic.
Absorption, Fate, Excretion :
Adverse / Side Effects :
Preparation / Dose :
|
Drug |
Trade name |
Dose |
|
1. Streptomycin |
- |
0.5 – 2.0 g / I/M / day |
|
2. Kanamycin |
Kantres |
1 gm I/M / day |
|
3. Gentamicin |
Garamycin |
3 – 5 mg / kg / day / I/M |
|
4. Tobramycin |
Nebcin |
3 – 4 mg / kg/ day / I/M |
|
5. Amikacin |
Amikin |
15 mg / kg / day / I/M |
Clinical Application / Therapeutic Uses :
Contraindication / Interactions :
TETRACYCLINES AND OTHER ANTIBIOTICS
BROAD SPECTRUM ANTI-BIOTICS
Definition :
These antibiotics are not only effective against gm–positive and gram–negative organisms, but also rickettsiae, mycoplasmae, chalmydia and brucella. Hence, they are called Broad Spectrum Antibiotics.
TETRACYCLINE
Definition :
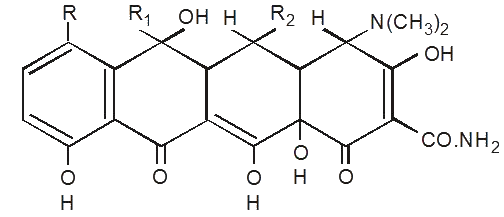
Tetracyclines are broad-spectrum antibiotics and are naphthalene derivative.
Antibacterial Spectrum :
Tetracyclines are effective against Gram-positive and Gram-negative organisms, including pneumococci, gonococci, clostridia, H.indluenzae, H.pertusis. H.ducreyi, Brucella, vibrio comma etc.
Mechanism of Action :
Tetracyclines act by inhibiting certain essential enzyme systems of bacterial cell. Tetracyclines are known to inhibit protein synthesis in bacterial ribosomes.
Tetracyclines bind with magnesium, manganese and calcium to form insoluble complexes ‘chelates’, and by removing these divalent metallic cations from sites, they inhibit enzyme activation.
Thus, tetracyclines are bacteriostatic in action.
However, in higher concentrations or parenteral administration, they may exert a bactericidal effect.
Absorption, Fate, Excretion :
Adverse / Side Effects :
Preparation / Dose :
|
Drug |
Trade name |
Dose / route |
|
Chlortetracycline |
Aureomycin |
|
|
Oxytetracycline |
Terramycin |
250 mg 6 hourly oral |
|
Tetracycline |
Achromycin |
|
|
Demethyl-chlortetracycline |
Ledermycin |
|
|
Methacycline |
Rondomycin |
150 mg to 300 mg 6 hourly oral |
|
Doxycycline |
Vibramycin |
|
|
Minocycline |
Minocin |
150 mg to 300 mg 6 hourly oral |
|
Rollitetracycline |
Reverin |
|
Clinical Applications / Therapeutic Uses :
Contraindication :
Interaction :
CHLORAMPHENICOL
Definition :
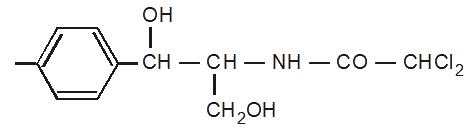
It is a broad-spectrum antibiotic derived from streptomyces venezuelae.
Antibacterial Spectrum :
Chloramphenicol is a broad-spectrum antibiotic, effective against Gram-positive and Gram-negative bacteria, chlamydia, rickettsiae, salmonella typhie etc.
Mechanism of Action :
Chlorampenicol acts by inhibiting bacterial protein synthesis. It is a bacteriostatic agent.
Absorption, Fate, Excretion :
Adverse Effects :
Preparation / Doses :
|
1. Chloramphenicol (tablet) |
250 mg capsule / oral 1.5 to 3.0 gm dose. |
|
2. Chloramphenicol palmitate (suspension) |
125 mg / ml for paediatric use 50 mg / kg (body wt.) / day dose |
|
3. Chloramphenicol sodium succinate (injection) |
1 gm vial 50 mg / kg (body wt.) / day dose |
Clinical Application / Therapeutic Uses :
Note :
Contraindications :
〄〄〄